 They are concerned about the renal function of a 43 year old woman who is day 26 post allogenic stem cell transplant for relapsed Acute Myeloid Leukaemia (conditioning with alemtuzumab, melphalan and fludarabine).
They are concerned about the renal function of a 43 year old woman who is day 26 post allogenic stem cell transplant for relapsed Acute Myeloid Leukaemia (conditioning with alemtuzumab, melphalan and fludarabine).
Her pre-transplant renal function was normal (creatinine around 60umol/L, eGFR>60ml/min), but has been on a pattern of fluctuating deterioration since around day 5 post transplant, reaching a level today of 415umol/L, eGFR 10ml/min, Urea 17.9, K+ 4.3, Na 143, HCO3 18). Initial declines co-incided with episodes of sepsis and i.v Gentamicin use. The patient has also been on Cyclosporin A microemulsion as prophylaxis against graft-versus-host disease, and has had a series of high serum trough levels (generally >300, target <200). Cyclosporin has now been discontinued and replaced with Tacrolimus, with an initial trough of 15.1, and a Cyclosporin level which is still high at 220. Her weight is currently down 7kg from initial admission, and fluid balance demonstrates ongoing high (2-3L/day) urine output, with around 2L/day oral intake.
Case contributed by David Ferenbach.
What results would you like to see immediately? Think carefully before clicking.
Further information
- Platelets have been consistently low (<20).
- Blood film 2 days ago showed no evidence of red cell fragmentation.
- Renal tract USS showed normal sized unobstructed kidneys.
- Urine dipstick +haematuria, no proteinuria.
- MSU – growing yeasts (further classification pending).
Now consider what advice you would give.
Expert review
Cause: is not certain. As often in AKI there are a number of plausible causes or exacerbating factors, but here they are particularly numerous.
- Volume depletion. Falling weight & high urine output would be consistent with this. Impaired concentrating ability leading to a high obligate urine output can be a feature of both aminoglycoside toxicity and acute interstitial nephritis
- Urinary sepsis. This will deliver an additional renal ‘hit’ and it is of note further treatment for a fungal urinary tract infection is needed.
- Acute Interstitial Nephritis. The patient has been exposed to multiple courses of antibiotics over the preceding 4 weeks, which would be the most likely trigger & is also on a proton pump inhibitor.
- Aminoglycoside Toxicity. Gentamicin was administered earlier in the clinical course- it seems unlikely this is the sole cause of the current problems but could be a sensitizing factor to other insults.
- Calcineurin Toxicity. The patient currently has supra-therapeutic and potentially toxic levels of two calcineurin inhibitors at the same time, which have both haemodynamic and tubulotoxic effects on the kidney.
- Thrombotic Microangiopathy. Chemotherapy, malignancy and CNIs are all associated with the development of a renal TMA. This is associated with low platelets, although in this patients case the low platelets have persisted since her induction chemotherapy, and the absence of red cell fragments is against this diagnosis (as is the lack of blood+protein in the urine dipstick).
Advice: Efforts should be made to address reversible factors in the above differential. Ensure fluid replete and aim for net positive fluid balance over the coming weekend. Treat sepsis.
For renal function it would be desirable to reduce exposure to calcineurin inhibitors (Cyclosporin, Tacrolimus), and this should be discussed with her haematology/oncology team.
Suggest repeating blood film with particular attention to features of TMA on blood film, and checking LDH (raised in intravascular haemolysis).
Monitor renal function daily. Renal replacement therapy would be appropriate if required. Diagnostic renal biopsy may be desirable, although the current platelet count makes that a harder proposition.
Further info:
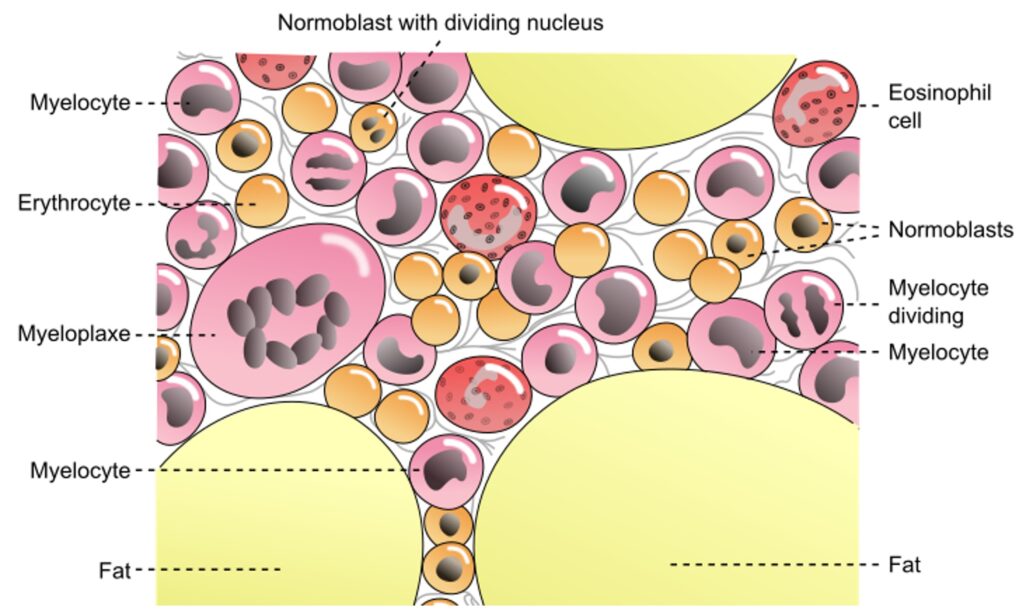
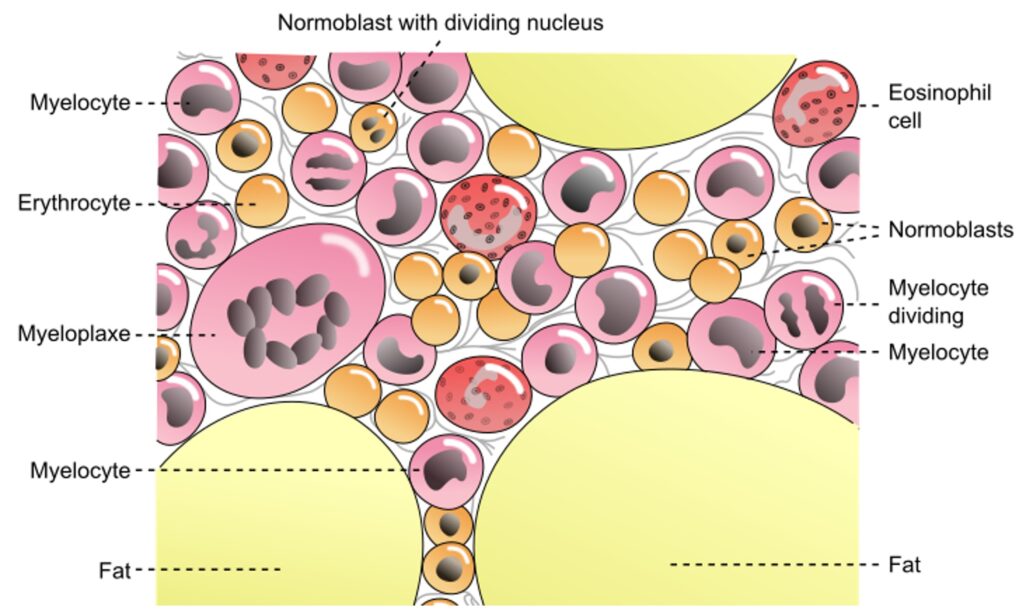
Image: Diagrammatic view of normal bone marrow via openstax at Wikimedia Commons
Last Updated on February 9, 2025 by admin
 They are concerned about the renal function of a 43 year old woman who is day 26 post allogenic stem cell transplant for relapsed Acute Myeloid Leukaemia (conditioning with alemtuzumab, melphalan and fludarabine).
They are concerned about the renal function of a 43 year old woman who is day 26 post allogenic stem cell transplant for relapsed Acute Myeloid Leukaemia (conditioning with alemtuzumab, melphalan and fludarabine).